
Tick Centre
Here at medica, we offer a full laboratory screening service for diseases associated with ticks.
Nowadays, ticks can be found almost anywhere in Switzerland up to an altitude of around 2,000 metres. They mainly live in deciduous forests with abundant undergrowth. Ticks infected with viruses can transmit pathogens to humans when they bite – infections such as tick-borne encephalitis (TBE) and Lyme disease, in particular, have increased significantly in recent years.
TBE and Lyme disease
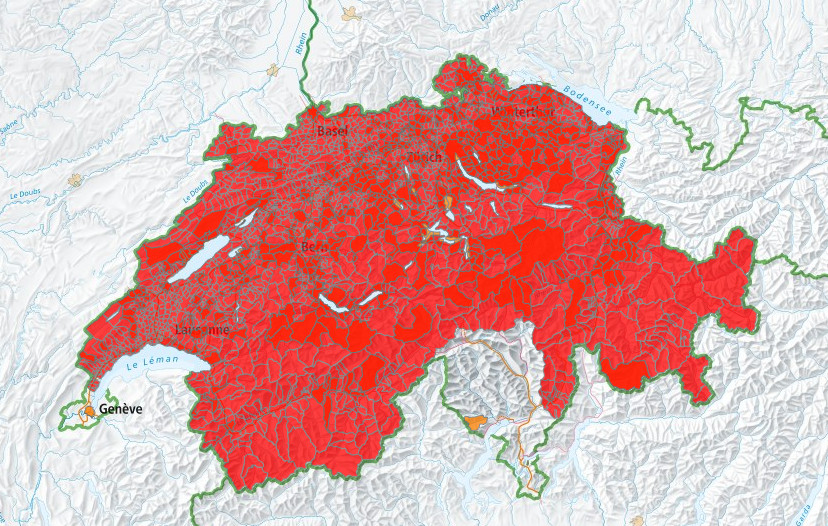
According to the FOPH, 243 people in Switzerland fell ill with tick-borne encephalitis (TBE) betweeen January and June 2023. In the years since 2000, between 48 and 409 cases have been registered in the same period. An effective course of treatment does not exist, which is why anyone who travels to TBE risk areas (red) or spends a lot of time in the outdoors is advised to be immunised against TBE.
Significantly more people also visited a doctor due to tick bites or Lyme disease. By the end of June, around 21,300 visits to a doctor had been made for tick bites and 6,900 for acute cases of Lyme disease. After diagnosis, Lyme disease can be treated effectively with antibiotics. In cases of acute infection, the antibodies cannot be detected until 2-3 weeks after contact. There is no need to examine the tick. A serum tube is required for the analysis. CSF is examined only in clinically inconclusive and severe cases.
Figure above: TPE vaccination recommendation issued by the FOPH in 2020
Laboratory tests
TBE (tick-borne encephalitis)
- Successful vaccination, contact made: evidence of IgG antibodies
- Acute infection: evidence of IgM antibodies
- PCR = direct evidence of pathogen
Lyme disease
- Screening test (EIA)
- Further specific antigens in the IgG/IgM western blot test
- PCR
Suspected neuroborreliosis (CSF and serum required)
Typical pattern in basic diagnosis-specific Borrelia IgG and IgM antibodies
Other: Rickettsia, Babesia, tularaemia

Meat allergy
Occurrence and incidence
Meat allergies are rare. A person may develop a meat allergy after being bitten by a tick. This primarily affects young people/adults with no history of allergies.
Sensitisation
If you are bitten by a tick, alpha-gal is transferred from the tick’s saliva into your blood. As a result, the immune system forms antibodies against alpha-gal to neutralise it, including IgE antibodies. Sensitisation to alpha-gal can trigger an allergic reaction when a patient eats meat.
Alpha-gal is found in:
- The meat of mammals such as beef, pork, lamb and game, and offal such as kidney; the larger and fattier the piece of meat being consumed, the more likely it is for an allergic reaction to occur.
- Gelatine from mammals (for example in desserts, jelly sweets and medical infusions)
Clinical manifestation
Reactions generally occur 3-6 hours after consuming meat:
- Urticaria
- Gastrointestinal complaints (stomach ache, diarrhoea)
- Anaphylaxis
Laboratory tests
- ImmunoCap Pork (f26), Beef (f27) and Mutton (f88)
if positive - ImmunoCap alpha-gal (o215)
Diagnosis is confirmed by IgE against the meat of different mammals.
IgE against alpha-gal is higher than IgE against the meat of mammals.

Rabbit fever/tularaemia
Tularaemia is an infectious disease which is transmitted in a variety of ways, including through tick bites. The number of cases recorded in Switzerland has been on the rise since 2015
Clinical manifestation
linical pictures 3 to 5 (21) days after infection can differ. Initial flu-like symptoms with fever are followed by ulcerative inflammation at the point of entry with swelling of regional lymph nodes, pneumonia, colitis and sepsis. A special form of the disease manifests as conjunctivitis with preauricular lymph node swelling. The outcome can be fatal in 5-15% of cases if left untreated. Early intervention with antibiotics such as ciprofloxacin or doxycycline, in combination with aminoglycosides (gentamicin, streptomycin, etc.) if required, reduces mortality to virtually zero.
Transmission
Highly contagious zoonotic diseases. They are transmitted through tick and insect bites, drinking contaminated water, eating insufficiently cooked meat of contaminated wild animals and inhaling contaminated water or hay dust. These diseases cannot be transmitted from one human to another.
Diagnosing Francisella tularensis
Serum antibody test: immunoassay for IgG and IgM
Detection of pathogens in the blood, lymph nodes, pus, ulcer swab, tick: culture, PCR
Your contact persons
PD DrAxel Regeniter
Head Infectious Disease Serology/Immunology
Specialist in Laboratory Medicine, Multidisciplinary FAMH
Clinical Chemistry and Immunology, Protein and CSF Diagnostics
PD DrWerner Siede
Deputy Head Infectious Disease Serology/Immunology
Specialist in Laboratory Medicine
Proteins, Enzymes, Lipids and Nutritional Physiology

